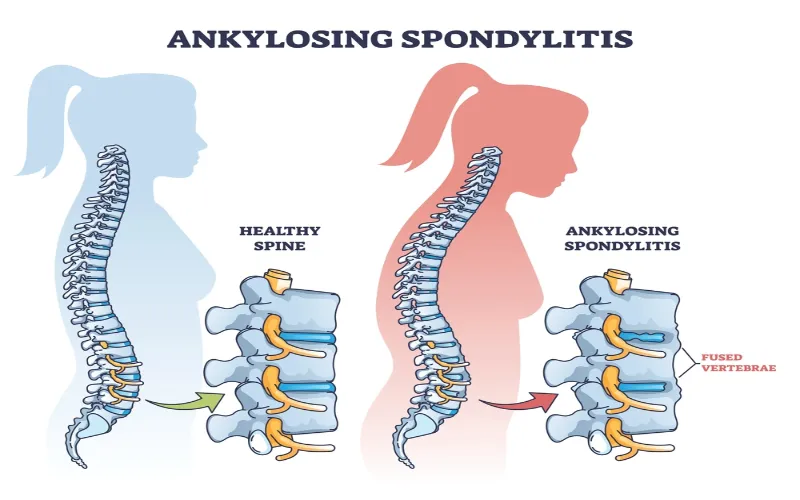
Ankylosing spondylitis is an inflammatory disease that ultimately results in the fusion of spinal vertebrae. Fusing the vertebrae makes the spine more rigid and less flexible, resulting in a hunched posture. It is known that ankylosing spondylitis is an autoimmune disease. However, it turns out that it may also be driven by the human microbiome.
In the rapidly expanding world of medical research, “Ankylosing Spondylitis Human Microbiome” stands out as a groundbreaking topic of interest. It represents the compelling intersection between Ankylosing Spondylitis, a chronic inflammatory condition primarily affecting the spine, and the vast universe of the human microbiome, which consists of trillions of microorganisms playing pivotal roles in our health and well-being. As researchers delve deeper into this connection, understanding how the human microbiome might influence or be influenced by Ankylosing Spondylitis offers transformative potential for diagnostic and therapeutic approaches.
Defining the Human Microbiome
The human microbiome represents a symbiotic community of microorganisms living in our body. This complex ecosystem is characterized by bacteria, viruses, fungi, protozoa, archaea, and eukaryotes, each serving distinct roles.
Distribution across the Human Body
Microbes are omnipresent in the human body. From the mucosal linings of the respiratory and urinary tracts to the surface of our skin and mouth, microbial communities are found everywhere, maintaining a delicate balance with their host.
Ankylosing Spondylitis: A Brief
Ankylosing Spondylitis (AS) is a chronic inflammatory disease predominantly affecting the spine. Recent studies have shed light on the role the human microbiome, particularly gut microbiota, may play in its onset and progression.
The Disease Pathogenesis
AS is linked with inflammation, leading to spinal joint pain and stiffness. The exact etiology remains a research subject, but increasing evidence points towards microbial imbalances in its development.
Gut Microbiota’s Role in AS
The gut, a primary site for bacterial colonization, showcases interactions between the host and pathogens or microbes. Alterations in gut microbiota have been linked with AS, suggesting a relationship between gut health and disease progression.
Investigating the Connection
The interface between the human microbiome and AS has ignited many questions. Comprehensive studies and analyses are being conducted to decode this relationship further.
Recent Studies and Findings
Recent human microbiome project research has analyzed the composition, diversity, and genes of the microbial communities in AS patients. Preliminary findings indicate a shift in gut microbiota, with certain bacteria types being predominant.
Therapeutic Applications
Harnessing the information about microbial differences in AS patients, researchers are exploring therapeutic interventions. Modulating the human gut microbiome offers a promising approach to manage or possibly even prevent the disease.
Future Prospects and Challenges
The human microbiome’s dynamic nature and individual variations present opportunities and challenges. As we delve deeper into the microbial world, our understanding broadens, paving the way for innovative treatments.
Microbiome-based Therapies
With the identification of specific microbial communities associated with AS, microbiome-based treatments are on the horizon. Probiotics, diet, and other methods may soon become part of AS management strategies.
Challenges in Research and Application
The vast number of microorganisms, their complex interactions, and the influence of external factors like diet and environment make human microbiome research challenging. Moreover, ensuring the safety and efficacy of new treatments is paramount.
Latest Research Findings
Another study was also done to analyze the unique gut microbiome biomarkers seen as ankylosing spondylitis progresses. Patients with ankylosing spondylitis were found to have increased amounts of Prevotella melanogenic, Prevotella copri, and Bifidobacterium, while they had decreased amounts of Bacteroides. It is suggested that these alterations in the microbiota participate in the pathogenesis of ankylosing spondylitis. A potential treatment may arise out of the microbiome.
Wen, C., Zheng, Z., Shao, T., Liu, L., Xie, Z., Chatelier, E. L., . . . Ehrlich, S. D. (2017, July 27). Quantitative metagenomics reveals unique gut microbiome biomarkers in ankylosing spondylitis. Retrieved from https://genomebiology.biomedcentral.com/articles/10.1186/s13059-017-1271-6
What are microbiome-based therapies?
These treatments target the human microbiome, like using probiotics or modifying diet to manage diseases such as AS.
What challenges exist in microbiome research?
Researching the microbiome is challenging given the vast number and complexity of microorganisms, their interactions, and influences like diet.
Can probiotics help AS patients?
As part of microbiome-based treatments, probiotics might become a key component in AS management strategies.




